CDC To Gay Porn Stars: You Should Be On Truvada
 In 2014, a bareback gay porn star who was unknowingly HIV-positive passed the virus on to one of his co-stars during production of a bareback gay porn scene in Nevada. Now, that single transmission of HIV is the impetus for a study in the CDC’s Morbidity and Mortality Weekly Report, released today.
In 2014, a bareback gay porn star who was unknowingly HIV-positive passed the virus on to one of his co-stars during production of a bareback gay porn scene in Nevada. Now, that single transmission of HIV is the impetus for a study in the CDC’s Morbidity and Mortality Weekly Report, released today.
This report gets extremely detailed, as they tracked down just about everyone with whom the performer had sex, and they were able to determine how and when the virus was transmitted using genetic testing. The study also proves that HIV testing, while certainly reliable, is not enough to prevent the spread of HIV, given so-called “window periods” when a positive performer can still test negative for the virus.
Excerpts from the CDC’s report:
In 2014, the California Department of Public Health was notified by a local health department of a diagnosis of acute human immunodeficiency virus (HIV) infection* and rectal gonorrhea in a male adult film industry performer, aged 25 years (patient A). Patient A had a 6-day history of rash, fever, and sore throat suggestive of acute retroviral syndrome at the time of examination. He was informed of his positive HIV and gonorrhea test results 6 days after his examination. Patient A had a negative HIV-1 RNA qualitative nucleic acid amplification test (NAAT)† 10 days before symptom onset. This investigation found that during the 22 days between the negative NAAT and being informed of his positive HIV test results, two different production companies directed patient A to have condomless sex with a total of 12 male performers. Patient A also provided contact information for five male non–work-related sexual partners during the month before and after his symptom onset. Patient A had additional partners during this time period for which no locating information was provided. Neither patient A nor any of his interviewed sexual partners reported taking HIV preexposure prophylaxis (PrEP). Contact tracing and phylogenetic analysis of HIV sequences amplified from pretreatment plasma revealed that a non–work-related partner likely infected patient A, and that patient A likely subsequently infected both a coworker during the second film production and a non–work-related partner during the interval between his negative test and receipt of his positive HIV results.
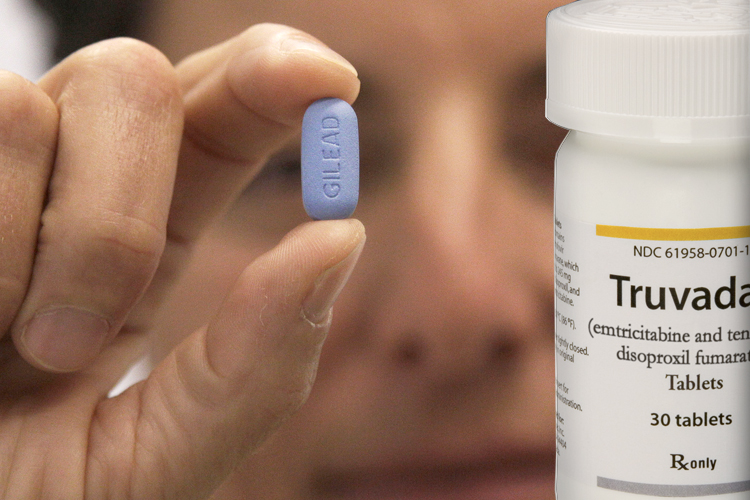
The CDC’s surprising conclusion and suggestion is that, based on this single transmission of HIV on a bareback porn set, all performers should be on Truvada/PrEP:
Adult film performers and production companies, medical providers, and all persons at risk for HIV should be aware that testing alone is not sufficient to prevent HIV transmission. Condom use provides additional protection from HIV and sexually transmitted infections (STIs). Performers and all persons at risk for HIV infection in their professional and personal lives should discuss the use of PrEP with their medical providers.
Obviously, a production company (or any business/employer) can not in any way regulate their employees or contractors’ prescription drug use, and anyone who suggests that they can or should be able to is clearly insane. Just imagine the lawsuits if a studio was in any way responsible for monitoring porn stars’ PrEP use, and then one of those porn stars ended up becoming HIV-positive.
Also, it’s still bizarre to me that a porn studio can legally inform its models about who is HIV-positive, but I assume the positive performers gave their consent to have their statuses disclosed. More from the report:
During the first production (a 1-day film shoot on the day before his symptoms began and 9 days after his negative NAAT), Patient A had condomless insertive and receptive anal sex with two HIV-negative performers (contacts 1 and 2) and condomless receptive and insertive oral sex with four HIV-infected performers (contacts 3–6). Patient A reported that the production company informed him before the film shoot that contacts 3–6 were HIV-infected with undetectable viral loads. During the second production (a 3-day film shoot that began the day after patient A’s symptom onset and 11 days after his negative NAAT), patient A had condomless receptive and insertive oral sex and condomless insertive anal sex with three HIV-negative performers (contacts 7–9), and condomless receptive and insertive oral sex with three HIV-negative performers (contacts 10–12).
After obtaining consent from patient A, local health department staff contacted the two production companies and obtained contact information for each of his work-related sexual partners. The performers and patient A’s non–work-related sexual contacts lived in seven U.S. states and four foreign countries. The production companies were based in two other states, and filming occurred in yet another state. The local or state health department of each performer confidentially notified all eight performers previously known to be HIV-negative, two performers previously known to be HIV-infected, and all five named non–work-related sexual partners to inform them of their potential HIV and gonorrhea exposures. Two other performers previously known to be HIV-infected could not be located. All persons contacted were offered immediate and follow-up (30-day) HIV NAAT and STI testing. Pre-treatment plasma was collected from patient A and all his contacts with newly diagnosed HIV infections. Using established methods (1), HIV-1 polymerase (pol; 997-bp) and p17 gag (gag; 411-bp) sequences were independently polymerase chain reaction–amplified from plasma specimens.
Among patient A’s work-related sexual contacts from the first film production, contacts 1 and 2 had negative HIV NAATs 62 and 53 days after filming, respectively, indicating that patient A did not infect any work-related sexual contacts from the first film production. Contact 4 received a diagnosis of early latent syphilis 13 days after filming, and contact 2 received a diagnosis of genital chlamydia infection 23 days after filming. No evidence of prefilming HIV testing was made available to investigators from this production company.
Among patient A’s work-related sexual contacts from the second film production, contact 7 (hereafter referred to as patient B) experienced fever and sore throat suggestive of acute retroviral syndrome 4 days after filming concluded, and received a diagnosis of acute HIV infection 18 days after filming.
The CDC report concludes with another push for PrEP, which is fine for individuals who choose to go on the drug but, again, insane to suggest that an employer can mandate or regulate use:
Persons at high risk for HIV infection should receive periodic HIV and STI testing.*** However, as demonstrated here and previously among heterosexual adult film performers (2), testing alone is not sufficient to prevent occupational HIV transmission. HIV can be transmitted during the 14-day period after a negative NAAT test, before a positive test is obtained. PrEP significantly reduces the risk for HIV acquisition among HIV-negative persons at high risk; however, PrEP is not an intervention with which employers can ensure compliance, and should be used with condoms to protect against both HIV and other STIs.
There, at least the CDC acknowledges that employers can’t ensure compliance (and that PrEP does absolutely nothing to protect against other diseases). But then, one sentence later, they say the adult industry should “consider” implementation of PrEP, a prescription drug. The fuck?
The high prevalence of STIs within this network of sexual partners, including performers, emphasizes the importance of consistent condom use. In addition to complying with regulatory requirements under OSHA standards, the adult film industry should consider the implementation of combination HIV prevention strategies, including biomedical (HIV testing, treatment, and PrEP) and behavioral (consistent and correct use of condoms) interventions.
Again: Insane. And probably illegal.